By the time that a young Dr Charles Fletcher, based at the Radcliffe Infirmary in Oxford, became the first physician ever to treat a patient with antibiotics, the use of militaristic “War on Germs” language had already dominated medical discourse for decades. The isolate-and-destroy, “us versus them” approach to fighting disease-causing microbes was widely accepted, and this mindset, along with the rapid rise in the use of antibiotics, has been a major force in leading medicine to where it is today. We have seen an astounding drop in worldwide mortality which has rendered antibiotics arguably one of the greatest advancements in human history. Yet the rise of bacterial resistance and the complexity of diseases like hepatitis and HIV/AIDS has also helped us to realise that solutions to most diseases are much more complicated – and may need to be much more personalised – than previously thought.
The notion that microbes residing in our bodies could be “healthy” existed prior to the discovery of antibiotics. In the early 19th century, Russian researcher Elie Metchnikoff noticed a pattern of longer lifespans among certain Bulgarian peasant populations who consumed large quantities of fermented dairy products containing lactic acid-producing bacterial species. He hypothesised that high consumption of these bacteria crowded out more “toxic” strains of bacteria in the gut that were contributing to the aging process. Not only did his research prompt Metchnikoff to drink sour milk every day for the rest of his life in order to reverse aging, but it also triggered more work in the area of “healthy microbes”. This was a line of research that – although somewhat obscured during the 20th century by major discoveries like antibiotics – has re-emerged as new challenges like the rise of antibiotic resistance have forced us to frantically look toward new disease-solving approaches. It has prompted us to re-focus our efforts on achieving ecological balance rather than microbial obliteration.
In 2001, during the wave of triumph produced by the publishing of the first human genome sequence, American molecular biologist Josh Lederberg coined the term “human microbiome” to represent the microbial community – including the good, bad, and neutral micro-organisms – living in and on us. Lederberg was one of a group of scientists who argued that reaping the full benefits of the mapped human genome was impossible without better understanding the dynamic relationship, including the complex genetic interactions, between our own bodily cells and the micro-organisms living with us.
Growing recognition of the need for more knowledge in this area culminated in the launch of the Human Microbiome Project, in 2008. The international initiative encompasses the efforts of over 200 researchers who have begun the pain-staking work of cataloguing and understanding the micro-organism communities within us. Not only has the proliferation of studies in this area shed new light on human health and disease mechanisms, but it has fuelled support for a paradigm-shift in medical practice. It has helped us to recognize the ambiguities in how we view germs in relation to our own bodies and forced us to question both what we view as “healthy” and what we define as “us”.
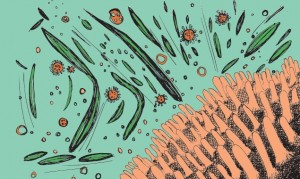
The picture that now emerges is one in which our bodies are dynamic ecosystems, replete with – and in some cases benefiting from – colonies of micro-organisms interacting with our bodies’ cells, our environments, and each other. This collection of resident organisms, which include bacteria, fungi, Archaea, viruses, and single-cell eukaryotes, comprises the “microbiome”. Consideration of the numbers involved is mind-boggling. Resident bacteria alone outnumber our own bodily cells by ten to one (there are an estimated 100 trillion “good” bacteria living in us) and account for about a pound of our body weight. Thousands of different strains of bacteria inhabit various sites in places like the skin, urogenital tract, oral cavities, and nasal passages, with the gut being the most densely populated region.
While our own genomes contain only about 20,000 genes (which seemed a surprisingly low number at the time it was determined), these genes are constantly exchanging information with our microbial “metagenome” which may collectively contain a hundred times more genes than that. Microbes are now thought to contribute more genes important for human health than a human’s own genes. Within minutes of being born, babies are colonised by microbes in the mother’s vagina, breast milk, and the external environment. This early period of colonisation is critical. By the end of the first few years of life, each person has developed a unique core microbial “profile” which is carried throughout life and can adjust to a certain extent with age, disease state, and environmental factors. This microbial profile also varies according to where a person lives: recent studies comparing the fecal microbiota of healthy children in Bangladesh and in the United States found significant differences between the two groups, with Bangladeshi children containing much greater microbial diversity and much less stable month-to-month structure than American children. The relative contribution of environmental, genetic, and medication-related factors (like antibiotic use) to such differences is an interesting question.
In 2012, the Human Microbiome Project reached a milestone, with the successful characterisation of the bacterial communities in various parts of the body for 242 healthy people in the United States. The results showed that the human ecosystem is comprised of over 10,000 species, and that even among healthy people there is significant microbial diversity from person to person. While there has been some evidence that the gut microbiota might fall into distinct enterotypes, much like blood types, there is still a lack of consensus on this idea. There remains disagreement on the correct methods for accurately capturing this diversity.
The gut microbiome, which contains 70% of all the microbes in the body, is in itself an incredible “super organ” and prime example of how the microbiome plays a critical role in nearly all parts of basic human functioning. The composition of gut microbiota has been associated not only with diseases like inflammatory bowel disease and obesity but also with cardiovascular disease and cancer. Remarkably, studies involving the transplantation of gut microbiota from obese mice into non-obese mice have resulted in the non-obese mice actually developing features of obesity. Results of other studies suggest that the guts of obese people contain a lesser proportion of a certain “good” bacteria than the guts of lean people.
In addition, the gut microbiome has also been found to play an essential role in “educating” our immune system early in life and shaping immune responses to diseases like allergies and HIV. It plays a potentially significant role in our response to medications, and certain gut bacteria are known to produce compounds that are equivalent to pharmaceuticals currently being administered to humans. Remarkably, links have even been found between the gut microbiota and psychiatric outcomes via the brain-gut axis, forcing us to re-think the meaning of a “gut feeling”. Studies in rats have established the vital relationship between microbial colonisation and development of proper stress responses, and others have shown that this gut microbiota-brain communication can activate genes that influence personality and memory.
Compelling health-related findings from studies of the human microbiome extend beyond the study of bacteria, though research on other categories of life is far more limited. Changes in the “human virome”, the constellation of prokaryotes, eukaryotes and viruses that exist inside our bodies, has already been associated with diseases such as cystic fibrosis and diarrhoea. Similarly, the fungal component of the human microbiome, which includes strains of yeast in the gut, has potentially been linked to colitis in mice. One study even found the abundance of certain strains of methanogenic Archaea living in patients’ mouths to be significantly associated with periodontal disease.
These convincing links between the composition of the microbiome and human health and disease, combined with the potential to alter the microbiome, raise ample possibilities for the creation of new therapeutics. The administration of specific probiotics has shown efficacy in clinical trials for diseases like enterocolitis, and the probiotics industry has been booming for decades while marketing “healthy bacteria”-containing products ranging from yoghurt to chewing gum. However, important issues – like the difficulty of characterizing the bacteria included in probiotics, as well as the relative lack of understanding of what constitutes a “healthy microbiome” in the first place – raise safety concerns and render the evidence on the health benefits of probiotics “inconclusive”, according to the European Food Safety Authority in 2012. Fecal transplants have also already shown efficacy in randomized controlled trials for treating Clostridium difficile infection and are being tested for a variety of other gastrointestinal and non-gastrointestinal disorders.
Additionally, the idea that each person’s microbiome is as unique as their fingerprint opens the floodgate of possibilities for personalized medicine. Doctors in the future could diagnose and prescribe treatments (or even just diets) tailored to the make-up of one’s distinct microbiome. This line of thought has even extended to the world of social-networking. A German nonprofit recently launced MyMicrobes, a sort of microbial Facebook. For a fee, the site allows one to genetically sequence her or his gut bacteria and connect to a network of people with similar microbial profiles and diseases to discuss challenges and possible treatments.
While significant work has been done, real challenges – like the fact that most microbial communities are not culturable – still pose significant barriers in the quest to elucidate the functions of the microbiome. That said, increased collaboration between microbial ecologists and other disease experts and the creation of technologies and new metagenomic techniques have revolutionized this field of research. We are only now just beginning to see the picture. More research needs to be done to understand our relationship with the categories of life living in and on us. Yet taken together, these new findings seem to direct attention toward the same mystifying theme: while our body is our house, we are not the only ones living in it. Instead, we consist of communities, and “we” are a part of “them” just as much as they are a part of us.
![Bodily Bacteria By the time that a young Dr Charles Fletcher, based at the Radcliffe Infirmary in Oxford, became the first physician ever to treat a patient […]](/wp-content/uploads/2013/02/bacteria2-e1361997571365-620x300.jpg)